The circulatory system remains at risk
Cardiovascular disease includes heart disease, atherosclerosis (hardening of the arteries), thrombosis (clogging of the arteries), and stroke. It is the primary cause of death in developed nations. In the United States, cardiovascular disease accounts for more than 42% of all deaths .1 In 1995, it cost Americans an estimated $137.7 billion.1 If all forms of major cardiovascular disease were eliminated in the U.S., total life expectancy would rise by almost 10 years!1
About one in four Americans have one or more of the major cardiovascular disease risk factors1:
- 20% of American adults have high blood pressure.
- 28% of American men and 25% of American women smoke.
- 52% of adult Americans and 37% of those under age 20 have elevated cholesterol levels.
- 25% of American adults are sedentary, reporting no leisure-time physical activity.
Despite considerable advances in scientific understanding of the causes of cardiovascular disease over the past several decades, the established risk factors cannot fully explain its occurrence.2 High blood cholesterol, for instance, is an important risk factor, yet most people who’ve had heart attacks have normal cholesterol levels.2 Years of searching for cause-and-effect relationships helped define common risk factors, including high blood pressure, high blood cholesterol, cigarette smoking, age, gender, obesity, and sedentary lifestyle. However, as well-defined and well-researched as these risk factors are, they still account for only about half of the deaths attributed to cardiovascular disease.
For this reason, researchers have continued to look for better explanations of the causes of cardiovascular disease. This research has led to a broader understanding of the role of lipotropic factors, B-vitamins, and related nutrients in maintaining the health of the circulatory system.
Nutrients help keep blood vessels healthy
A low-fat, high-fibre diet goes a long way towards supporting heart health. Caring for your heart, however, means more than just watching your saturated fat and cholesterol. Scientific data shows healthful benefits for several foods, including fruits, vegetables, oatmeal, garlic, onions, fatty fish such as salmon, and red wine. Science also supports cardiovascular benefits for the following nutrients, obtained from diet and/or supplements:

- vitamin E
- fibre
- carotenoids
- flavonoids
- omega-3 fatty acids
- vitamin C
- magnesium
- folic acid
- vitamin B6
- vitamin B12
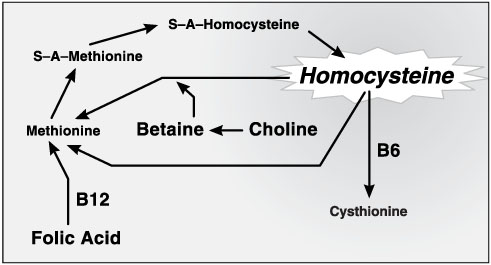
Nutrients support cardiovascular health through various mechanisms. For example, several nutrients participate in a biochemical pathway known as the “homocysteine cycle.” The lipotropic factor choline, plus the nutrients folic acid, vitamin B6, vitamin B12, and betaine all play crucial roles in the metabolism of homocysteine, an amino acid that can accumulate to dangerous levels and damage blood vessels. If deficiencies of these nutrients develop, the body cannot rid itself of toxic concentrations of homocysteine.
The homocysteine story
In 1966, Dr. Kilmer S. McCully made the initial observation that linked high blood levels of homocysteine to diseases of the blood vessels. Remarkably consistent findings from more than 20 research studies indicate that patients who have had strokes, heart attacks, or other forms of cardiovascular disease tend to have higher homocysteine levels than people without disease3:
- In Harvard’s Physicians Health Study, men whose homocysteine levels were in the highest 5% had triple the risk of having a heart attack compared to those with lower levels.4
- In a group of elderly Framingham Heart Study participants, narrowing of carotid arteries was twice as prevalent in those with the highest homocysteine levels compared to those with the lowest, after adjustment for sex, age, cholesterol, blood pressure, and smoking.5 The lower the folate and vitamin B6 levels, the greater the prevalence of narrowed arteries.
- In a baboon study, homocysteine infusions produced blood vessel damage within three months.3
High blood homocysteine may be the most consistent risk factor for heart disease… and high homocysteine levels are linked with dietary deficiencies of certain nutrients.
- The most common cause of high homocysteine levels is the deficiency of one or more key nutrients participating in the homocysteine cycle (folic acid, vitamin B6, vitamin B12).6,7,8
- Inadequate folic acid intake is the main cause of homocysteine-related damage to arteries.2
- A large proportion of the population, perhaps half, is not getting enough folate to keep homocysteine levels low.9
- In a study of apparently healthy men, 25% had low vitamin B6 levels, 57% had low vitamin B12 levels, and 59% had low folate levels.10 Homocysteine levels in turn were high. Daily supplementation with B-vitamins lowered homocysteine to normal levels within six weeks.
Normally, homocysteine is quickly converted to harmless products.13 But when essential components of homocysteine’s metabolic cycle are deficient, excess homocysteine can accumulate to dangerous levels.8 Many scientists believe homocysteine can injure artery walls, oxidize LDL (so-called “bad cholesterol”), and lead to the formation of artery-clogging plaques (atherosclerosis).7,12,13,14
Homocysteine Cycle
Research uncovers expanded lipotropic roles
The fats and fat-like substances in our bodies, including cholesterol, are broadly referred to as lipids. Lipids serve many important functions; they…
- provide the materials from which cell membranes are constructed.
- are metabolized as energy or stored for future energy needs.
- keep skin soft and pliable.
- support healthy glandular activity.
- insulate us from excessive cold.
- cushion and protect internal organs.
Lipids must be transported throughout the body in our blood before they can be utilized for these functions. Since blood is primarily water and fat is not water-soluble, lipids must be dispersed into fine particles and kept in this emulsified state in order to flow freely in the bloodstream. Lipoproteins are the substances that carry fine lipid particles in the blood, and lipotropic factors are essential for their synthesis.
In the early 1930s, researchers began to investigate the functions and mechanisms of lipotropic factors. They hypothesized that these factors were necessary for the mobilization of fat from the liver and other tissues that store fat. They showed in the laboratory that this was indeed the case. For instance, fat accumulated in the livers of experimental animals that were deficient in lipotropic factors, such as choline.
As early as 1979, GNLD first introduced the concept of supplementation of lipotropic factors with Lipotropic Adjunct.. This initial formula was improved in 1995 following several years of additional research, resulting in the advanced formula available today.
Lipotropic adjunct supports a heart-healthy blood environment
Lipotropic Adjunct is a leading-edge product intended for use in conjunction with a low-fat, high-fibre diet. It provides nutrients shown to play essential roles in maintaining the health of the circulatory system. Deficiencies of the essential participants in the homocysteine cycle can impede the breakdown of homocysteine, leading to its accumulation. GNLD’s special formula provides balanced amounts of lipotropic factors and other nutrients known to support the metabolism of homocysteine.
Bioavailable formulation includes betaine hydrochloride
Betaine - itself an important player in the homocysteine cycle - is delivered as betaine hydrochloride to supplement normal stomach secretions of hydrochloric acid, which aids the absorption of vitamin B12
Lipotropic factors assist transport and utilization of dietary fats
GNLD’s special Lipotropic Adjunct formulation provides concentrated lipotropic factors (choline and inositol) to help keep lipids emulsified in the blood, so they may be mobilized and utilized throughout the body where needed.
Citrus bioflavonoids
Bioflavonoids from oranges, lemons, and grapefruit support the health of the circulatory system. Research shows that citrus bioflavonoids, especially hesperidin, may relax blood vessels and favourably affect blood lipid levels.
References
(1) Heart and Stroke Facts: 1995 Statistical Supplement. American Heart Association. 1994. (2) Stampfer, M.J. Can Lowering Homocysteine Levels Reduce Cardiovascular Risk? New Engl. J. Med. 332:328–329, 1995.(3) Ueland, P.M., Refsum, H. and Brattstrîm, L. Plasma Homocysteine and Cardiovascular Disease. In: Francis, R.B., Jr., ed. Atherosclerotic Cardiovascular Disease, Hemostasis, and Endothelial Function. New York: Marcel Dekker, 183–236, 1992.
(4) Stampfer, M.J., Malinow, M.R., Willett, W.C., et al. A Prospective Study of Plasma Homocyst(e)ine and Risk of Myocardial Infarction in U.S. Physicians. JAMA 268:877–881, 1992.
(5) Selhub, J., Jacques, P.F., Bostom, A.G., D’Agostino, R.B., Wilson, P.W.F., Belanger, A.J. , O’Leary, D.H., Wolf, P.A., Schaefer, E.J. and Rosenberg, I.H. Association Between Plasma Homocysteine Concentrations and Extracranial Carotid-artery Stenosis. New Engl. J. Med. 332:286–291, 1995.
(6) Joosten, E., Van Den Berg A., et al. Metabolic Evidence that Deficiencies of Vitamin B12 (Cobalamin), Folate and Vitamin B6 Occur Commonly in Elderly People. Am. J. Clin. Nutr. 58:468–476, 1993.
(7) Selhub, J. and Miller, J.W. The Pathogenesis of Homocysteinemia: Interruption of the Coordinate Regulation by S-adenosylmethionine of the Remethylation and Transulfuration of Homocysteine. Am. J. Clin. Nutr. 55:131–138, 1992.
(8) Olszewski, A.J., Szostak, W.B., Bialkowska, M., et al. Reduction of Plasma Lipid and Homocysteine Levels by Pyridoxine, Folate, Cobalamin, Choline, Riboflavin, and Troxerutin in Arteriosclerosis. Atherosclerosis 75:1–6, 1989.
(9) Council for Responsible Nutrition. CRN News Supplement, April 21, 1995, p.1.
(10) Ubbink, J.B., Vermaak, W.J., Van der Merwe, A. and Becker, P.J. Vitamin B12, Vitamin B6 and Folate Nutritional Status in Men with Hyperhomocysteinemia. Am. J. Clin. Nutr. 57:47–53, 1993. (11) McCully, K.S. Chemical Pathology of Homocysteine. III. Cellular Function and Aging.
Ann. Clin. Lab. Sci. 24:134–152, 1994.
(12) Olszewski, A.J. and McCully, K.S. Homocysteine Metabolism and the Oxidative Modification of Proteins and Lipids. Free Radic. Biol. Med. 14:683–693, 1993.
(13) Cuinod, M., et al. Homocysteine, Folic Acid and the Prevention of Vascular Disease. Nutr. Rev. 47:247–249, 1989.
(14) Swendsed, M. Homocysteine, a Putative Pro-oxidant, and the Folate Requirement. Presented at the Western Human Nutrition Research Meeting on “New Approaches to Define Nutrient Requirements,” San Francisco, 1994.